The story follows Marcella Townsend, who was left unrecognisable by second and third degree burns she suffered after a propane explosion at her mother’s house in Georgia.
With few treatment options available, Marcella underwent a radical, cutting-edge procedure: a human placenta graft.
Incredibly, Marcella’s face now looks nearly identical to how it did before the explosion. [1]
What is a human placenta graft?
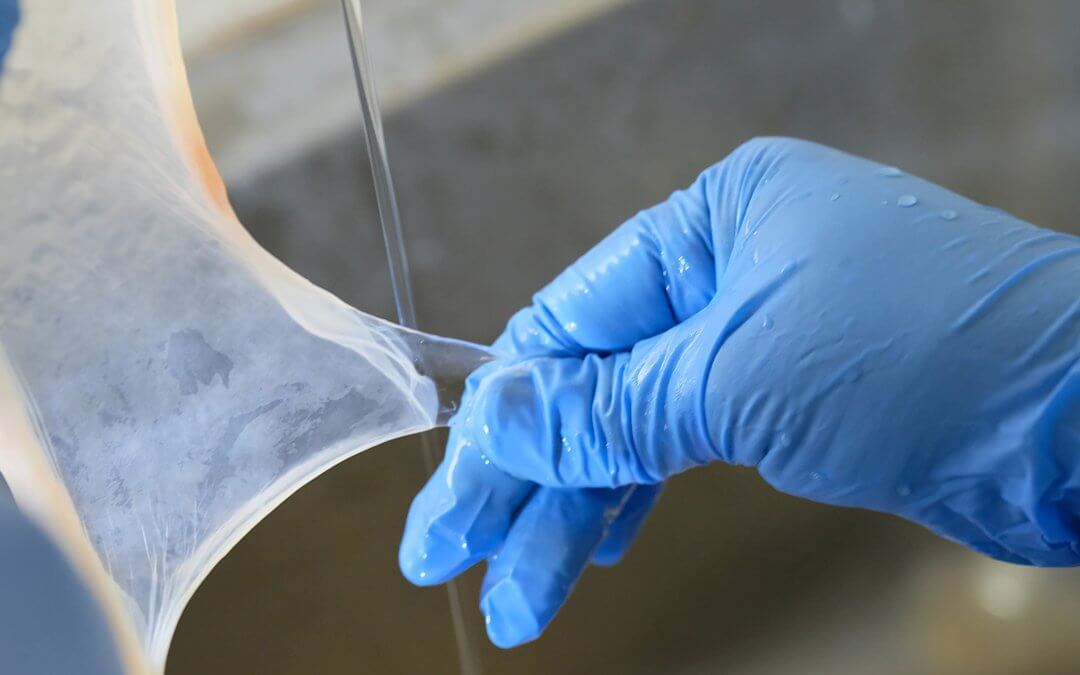
A placenta graft involves the application of amniotic membrane – the thin, translucent inner part of the placenta surrounding the foetus in the womb – to an area affected by burns, wounds, or injuries.
Unlike skin grafts using animals or cadavers, placental tissue doesn’t trigger the immune system, meaning it isn’t rejected by the body – a byproduct of the immunological privilege it has between mother and child during pregnancy.
It also stimulates rapid cell regrowth, which can help the body heal with minimal scarring. [2]
What makes the placenta so special?
The placenta provides crucial nutrients and protection to babies during pregnancy, and is filled with proteins and growth factors that make it extremely useful for healing injuries. [3]
Since the early 20th century, the amniotic membrane from placentas has been used in topical treatments for burns, wounds, and ulcers. It’s even been used to treat eye conditions. [4]
And yet, despite their potential, most placentas are discarded as medical waste.
Today in the U.S. only publicly stored donated placentas from elective C-sections are used. [1]
There are also limitations on how they can be used. For instance, amniotic membrane grafts are only sanctioned so long as there is minimal manipulation, meaning that their application is contained to internal and external bandages, along with cases of chronic wounds that take longer than usual to heal, or don’t heal at all.
In the latter context, a placenta graft again proved to be life-changing.
As cited by The New York Times, an 83 year old woman had an infected, chronic wound on her leg that wouldn’t heal after surgery. Having exhausted treatment options – including the use of larvae to eat the infected areas – doctors turned to placenta-derived skin grafts to close the wound.
The woman’s leg healed completely.
While the medical potential of the placenta seems boundless – they have been found to heal burns, wounds, and even restore vision in some cases – their lack of availability, along with the cost of associated procedures, means they remain vastly underused in the medical field. [1]
Why aren’t placentas more widely used?
While it’s clear that placentas have huge potential in a wide range of medical contexts, current therapeutic applications don’t come cheap. It is estimated that the cost of a placental graft ranges between $200 and $3,000 per square centimetre of amniotic membrane in the U.S. [1]
In the UK, amniotic membrane grafts are similarly pricey, with a document from the National Institute for Health and Care Excellence (NICE) showing a 2cm x 3cm graft costing around £1,000 for a single use. [5]
With the street worth of placentas estimated to be around $50,000 – a figure that’s expected to double or even triple over the course of the next decade [6] – it’s no wonder some mothers are looking to privately store their own placentas.
What is private placenta storage?
Private placenta storage is the process by which mothers can choose to store their placenta so that it’s available for their child to use in potential future therapies.
There are hundreds of clinical trials ongoing that are exploring the potential uses of placenta in treatments for conditions ranging from stroke to diabetes, Crohn’s and osteoarthritis. By saving the placenta, the powerful cells and growth hormones it contains are preserved for potential future use. [7] [8] [9] [10]
Private placenta storage can be considered to be part of what’s known as cord blood banking – the process by which the perinatal cells and tissues that naturally occur in the umbilical cord and placenta are cryogenically frozen.
Some of these perinatal cells are otherwise known as stem cells, and have many therapeutic benefits. Some are even being used today in over 80 approved treatments, mainly through the use of stem cells from a matched donor, such as a sibling.
Saving the umbilical cord and placenta for your baby may potentially give them access to any future therapies using stem cells and other perinatal cells and tissues, should clinical trials succeed and therapies become standard of care.
This is because cells from the umbilical cord and placenta are baby’s own perfect match, meaning that in therapies where autologous (the patient’s own) cells can be used, the risk of rejection in a procedure like a transplant is minimal.
For people like Marcella Townsend, the life-changing potential of the placenta is clear. By storing for your baby, you could help ensure that they too have access to this potential.
References
FIND OUT MORE, REQUEST YOUR WELCOME PACK TODAY
All you need to know to make an informed decision.
Provide your contact details to request:
– Complete Welcome Pack and Parent’s Guide
– Information via email
– Contact from our specialist advisors