Researchers are investigating a novel placenta-derived stem cell therapy for multiple sclerosis, a currently incurable degenerative neurological condition. A recent phase 1 clinical trial, with findings published in Scientific Reports, assessed the safety and feasibility of this approach for patients with secondary progressive multiple sclerosis.
What is multiple sclerosis?
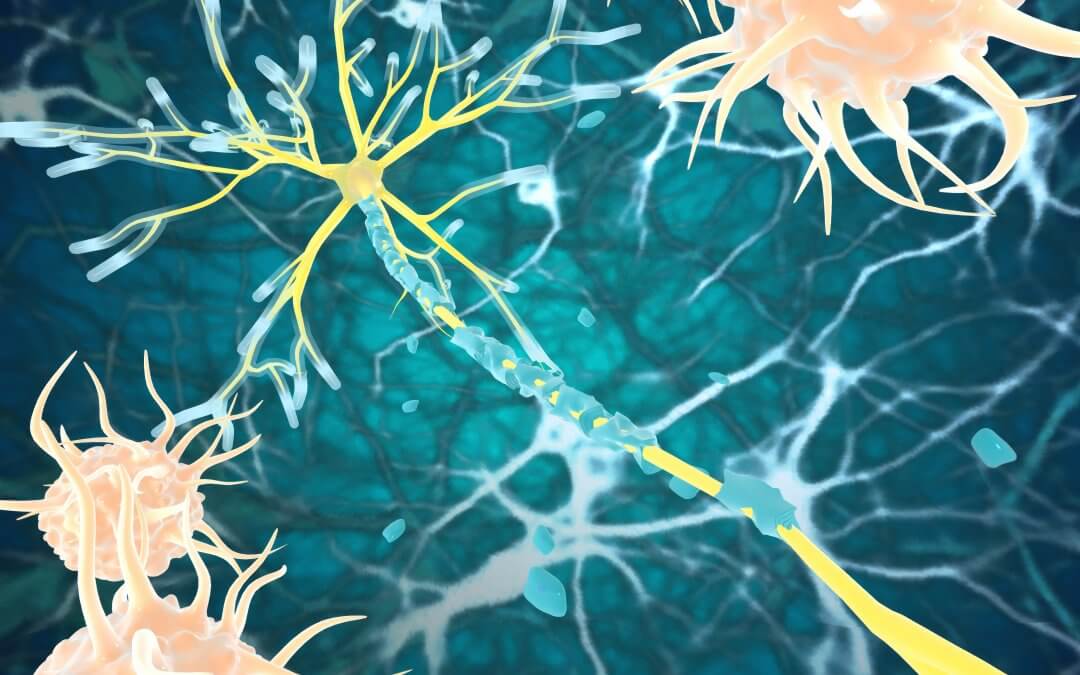
Multiple sclerosis is a lifelong condition that affects the brain and central nervous system. It is an autoimmune condition, caused by the immune system mistakenly attacking the myelin sheath which covers and protects the nerves. As a result of the myelin damage, the nerves become less efficient at sending messages to the body. The nerve damage continues to worsen over time, eventually leading to permanent disability.[1][2] Globally, multiple sclerosis affects around 2.3 million people.[3]
There are three main types of multiple sclerosis. In the relapsing-remitting type (RRMS), patients have distinct attacks (relapses) of symptoms, which then fade away partially or completely (remission). In the primary progressive type (PPMS), conversely, there is a gradual worsening of symptoms. Lastly, the secondary progressive type (SPMS) develops after RRMS for many people, and involves a gradual worsening of symptoms with or without active relapses.[4][5]
There is no cure for multiple sclerosis. Currently available treatment focuses on managing symptoms as well as reducing the seriousness and progression of the disease (disease-modifying therapies).[5][1]
Investigating stem cell therapy for multiple sclerosis
Current research is increasingly focusing on trying to find new treatments that would promote myelin regeneration (remyelination), reduce inflammation, and protect the nerves. Mesenchymal stem cells (MSCs) have the potential to address these goals, thanks to their anti-inflammatory, immunomodulatory, regenerative and neuroprotective properties. MSCs derived from the placenta (PL-MSCs), in particular, may have more potent immunosuppressive and immunomodulatory effects compared to other types of MSCs. What’s more, they can be obtained easily and non-invasively.[3]
Researchers posited that PL-MSCs may therefore have a positive impact on patients with SPMS, more specifically on those who no longer respond to conventional treatment (treatment-refractory).
The phase 1 clinical trial involved five patients with treatment-refractory SPMS, and was aimed primarily at determining the safety and tolerability of the PL-MSC treatment over a six-month period. Researchers also looked at exploratory secondary outcomes, including clinical disability, cognitive and psychological assessments, brain imaging (DTI and fMRI), and immunological markers.
What did the study find?
The treatment proved to be safe, with no serious complication occurring. Two patients had a mild headache, but this was resolved with a common painkiller.
Importantly, the results showed sustained improvements in clinical outcomes, with significant reductions in Expanded Disability Status Scale (EDSS) scores, a common measure of MS disability, in the first month after the treatment. By the third month, two participants had a continued reduction in their EDSS scores, while the other three remained stable.
After the treatment, participants also improved in cognitive and psychological tests. Functional MRI analysis suggested significant enhancements in brain connectivity and cognitive function. Blood tests also showed a decrease in the number of B cells, which are immune system cells involved in multiple sclerosis. Inflammatory proteins were found to have decreased, whereas anti-inflammatory protein levels increased.
The potential of placenta stem cells
It is important to keep in mind that this was a small phase 1 trial with a very limited number of participants, no control group and a relatively short follow-up period. The results are quite encouraging, but more research and larger-scale trials are needed to confirm the effectiveness of the treatment.
Nevertheless, studies like these highlight the strong potential of placenta stem cells, as well as other stem cells derived from birth-related tissues, to treat conditions and diseases that are currently considered incurable. Having ready access to a source of these powerful cells could make the difference in the future in terms of treatments that are still being discovered today. To learn more about how to bank your baby’s placenta and umbilical cord for their own future use, fill in the form below to receive your free guide.
References
[1] MS Trust (2022). What is MS? https://mstrust.org.uk/information-support/about-ms/what-is-ms
[4] MS Society (2019). Types of MS. https://www.mssociety.org.uk/about-ms/types-of-ms
[5] NHS (2022). Multiple Sclerosis. https://www.nhs.uk/conditions/multiple-sclerosis/
FIND OUT MORE, REQUEST YOUR WELCOME PACK TODAY
All you need to know to make an informed decision.
Provide your contact details to request:
– Complete Welcome Pack and Parent’s Guide
– Information via email
– Contact from our specialist advisors